Development and validation of a continuous measure of patient condition using the Electronic Medical Record
Rothman, Michael J. and Rothman, Steven I. and IV, Joseph Beals
Journal of Biomedical Informatics - 2013 via Local Bibsonomy
Keywords: dblp
Rothman, Michael J. and Rothman, Steven I. and IV, Joseph Beals
Journal of Biomedical Informatics - 2013 via Local Bibsonomy
Keywords: dblp
|
[link]
#### Goal: + Development and validation of a continuous score for patient assessment (to be used both outside and inside intensive care). + Prior work: Modified Early Warning Score (MEWS) identifies 44% of intensive care transfers occurring within the next 12 hours. Generates 69 false positives for each correctly identified event. #### Dataset: Model Creation | Model Validation ---------------|------------------ 22,265 patients admitted to the *Sarasota Memorial Hospital* (SMH) between Jan/2004 and Dec/2004 | 32341 patients admitted to the SMH between Sep/2007 and Jun/2009 | 45,771 patients admitted to the SMH between Jan/2008 and May/2010 | 32,416 patients admitted to *Abigton Memorial Hospital* (AMH) between Jul/2009 and Jun/2010 | 19,402 patients admitted between Jul/2008 and Nov/2008 in *Hospital C*. + ~ 7000 variables, 500 laboratory tests. + Constraints: + Variables should be related to the patient's condition + Collected with some frequency + Susceptible to variation during patient stay in the hospital + Focus: "How the patient is" not "Who the patient is" + The constraints reduce the number of candidate variables to 43 (13 nurse assessments, 6 vital signs and 23 laboratory tests) #### Rothman Index: + The Rothman Index is based on the "Excess Risk" associated with each of the variables: + The excess risk is determined by the increase (in percentage points) of the mortality at 1 year identified for that variable. In the best case, the "excess" risk is zero and the Rothman Index equals 100. 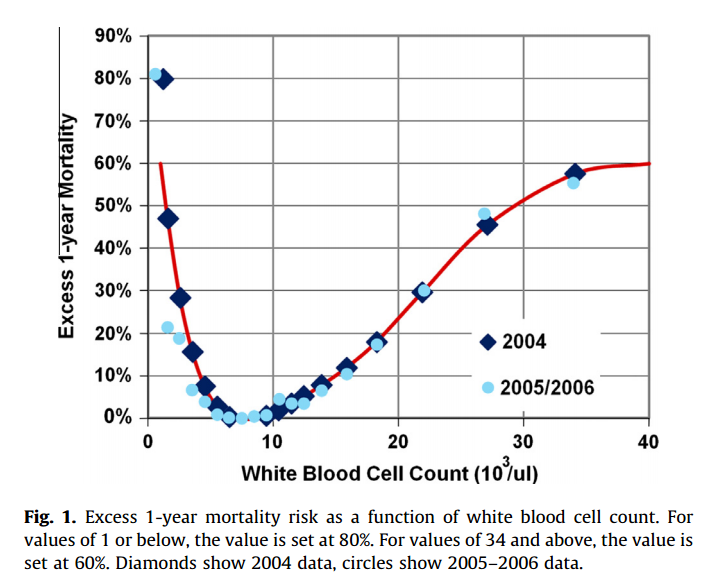 + The excess risk somewhat resembles the *impact coding* for categorical variables. One must always be careful that there is no data snooping. + The index consists of the 26 variables below. They were chosen from the 43 candidates using a *forward stepwise logistic regression* with the patients of the model creation dataset (criterion p-value <0.05). Note that the logistic regression is used only to choose the variables. The Rothman Index is not a regression model itself. 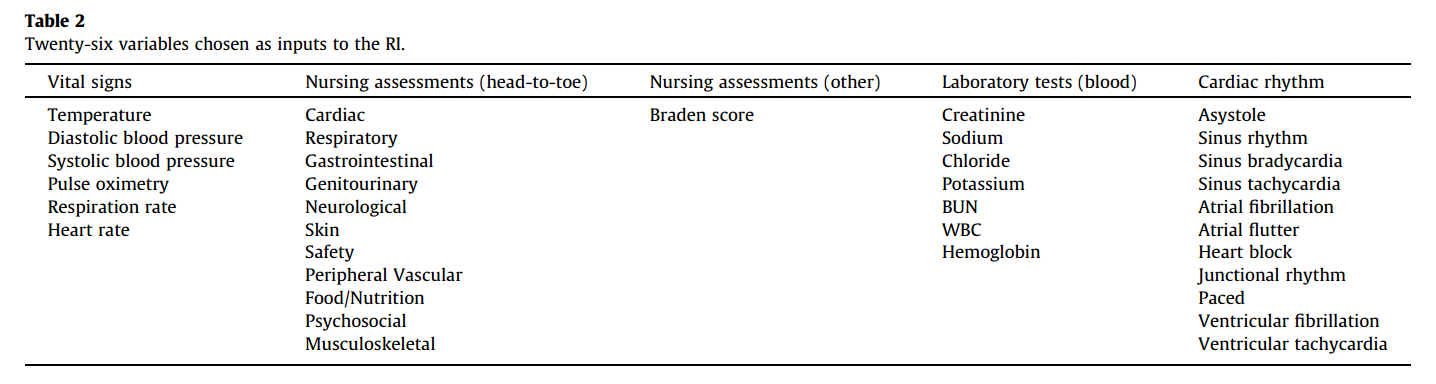 + The lab tests are collected less frequently. The score is divided into two parts (one that takes into account the laboratory variables and another that does not take into account). 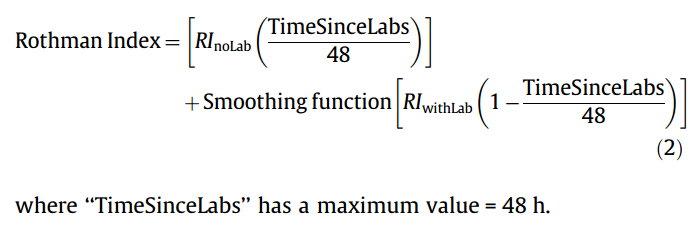 + *TimeSinceLabs* has a maximum value of 48 hours. #### Results: + Outcomes: + Mortality in 24h + Unplanned readmission in 30 days + Discharge + Rothman Index is correlated with discharge category (Home, Home healthcare, Rehab, Skilled Nursing Facility, Hospice, Death) |Mortality in 24h || Readmission in 30 days || Discriminates type of discharge| | |-------------|-|-----------------------|-|------------------------|-------------------------------| | Hospital| AUC | Hospital | AUC | Hospital | AUC| |SMH | 0.933 (0.915-0.930) | SMH | 0.62 (0.61-0.63) | SMH | 0.923 (0.915-0.930)| |AMH | 0.948 (0.960-0.970) | AMH | *| AMH | 0.965 (0.960-0.970)| |C | 0.929 (0.919-0.940) | C | *| C| 0.915 (0.900-0.931) | (*) in the case of readmission in 30 days it was possible to only identify the patients of the SMH hospital. + Tracking the Rothman Index and correlating it with events during hospital stay: 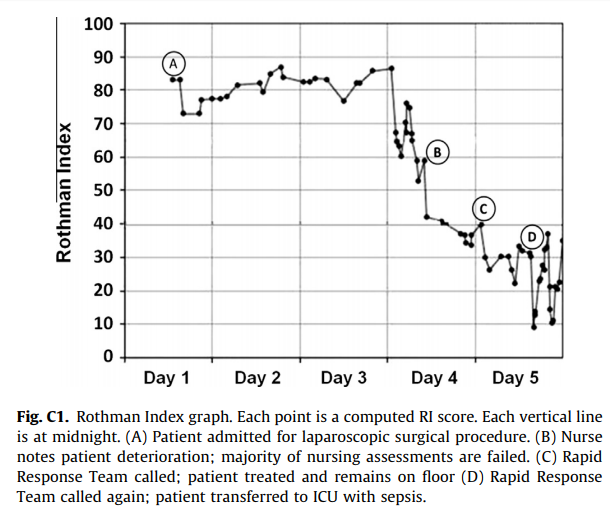 #### Discussion: + Choice of 1-year mortality to calculate excess risk: + Instead of in-hospital death, which is relatively rare (approximately 1—2% of patients), the model is based on 1-year post discharge mortality, where death is far more common (approximately 10% of patients). + Improve the *signal strength* to determine the relationships between clinical measures and risk. + Outcome should be sufficiently frequent and a plausible surrogate for the patient condition. In this case, the risk tries to quantify *distance from death*. + The Rothman index is not designed to predict any specific outcome. + Caveat: Results should have included precision/recall analysis. For risk assessment it is important to evaluate the rate of false alarms per one true positive. 
Your comment:
|
You must log in before you can submit this summary! Your draft will not be saved!
Preview:












